July 29, 2016
Promising Cancer-Fighting Gene Immunotherapy Could Be Used Against HIV, UCLA Research Suggests
EDGE null READ TIME: 4 MIN.
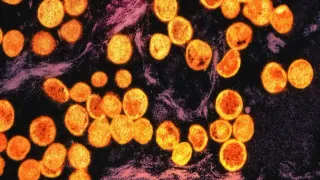
New UCLA research suggests that a gene-based immunotherapy that has shown promising results against cancer could also be used against HIV, the virus that causes AIDS.
�
In a study to be published in an August issue of the bi-monthly peer-reviewed Journal of Virology, researchers with the UCLA AIDS Institute and Center for AIDS Research found that recently discovered potent antibodies can be used to generate chimeric antigen receptors, or CARs, that can be used to kill cells infected with HIV-1.
�
CARs are artificially created immune T-cells that have been engineered to produce receptors on their surface that are designed to target and kill specific cells containing viruses or tumor proteins. The use of these chimeric receptors is currently the focus of gene immunotherapy against cancer, but they could also be used to create a strong immune response against HIV, said Dr. Otto Yang, professor of medicine in the division of infectious diseases at the David Geffen School of Medicine at UCLA and the study's corresponding author.
�
"We took new generation antibodies and engineered them as artificial T cell receptors, to reprogram killer T cells to kill HIV-infected cells," said Yang, who is also director of vaccine and pathogenesis research at the UCLA AIDS Institute and Center for AIDS Research. "Others have used antibodies against cancer antigens to make artificial T cell receptors against cancer and shown this to be helpful in cancer treatment. We are the first to use these new generation anti-HIV antibodies to design this strategy for HIV"
�
Although the human body's immune system does initially respond to and attack HIV, the sheer onslaught of the virus -- its ability to hide in different cells and to rapidly replicate -- eventually wears out and destroys the immune system, leaving the body vulnerable to a host of infections and diseases. Researchers have been looking for ways to strengthen the immune system against HIV, and it now appears CARs could be a weapon in that fight.
�
While the CARs approach has been in use for almost 10 years to fight cancer, this is the first application in HIV since failed trials 15 years ago, and different because it takes advantage of new antibodies that have been discovered in the past few years. In the previous trials, researchers had used an early type CAR that was not antibody-based. That approach, however, was abandoned because it was clinically ineffective.
Here the researchers used seven recently discovered, "broadly neutralizing antibodies" that have the ability to bind multiple strains of invading viruses, unlike earlier isolated antibodies that tend to bind few strains. These antibodies were re-engineered as artificial CAR-T cell receptors to have activity against broad strains of HIV. Testing them in the lab, the researchers found that all seven had varying degrees of ability to direct killer T cells to proliferate, kill, and suppress viral replication in response to HIV-infected cells.
Yang notes that "what works in a test tube doesn't necessarily work in a person," so the next step is to find strategies to put these receptors into humans. But this therapy shows enough promise to move forward with further research.
"All constructs have the ability to recognize infected cells for proliferation, killing and suppression of viral replication, although they may vary in their breadth of HIV-1 sequence diversity coverage," the researchers write. "Additional studies will be necessary to understand and assay the properties important for transduced cell proliferation and function for in vivo immunotherapies" using the broadly neutralizing antibody-based CARs.
Grants from the California Institute for Regenerative Medicine (#TR4-06845), the AIDS Healthcare Foundation, and the UCLA AIDS Institute and Center for AIDS Research funded this study.
Study co-authors are Ayub Ali, who was the lead author, Scott G. Kitchen, Irvin S.Y. Chen, Hwee L. Ng, and Jerome A. Zack, all of UCLA.